Everything You Need to Know About Cataracts Surgery
Understanding cataracts: A comprehensive overview
Cataracts are a common condition that can affect individuals, particularly as they age. They occur when the lens of the eye becomes cloudy, leading to decreased vision and an array of other visual disturbances. Understanding cataracts is vital in recognizing when one might need surgical intervention.
What are cataracts?
At its core, a cataract is a clouding of the natural lens of the eye. This lens is situated behind the iris and the pupil and is crucial for focusing light onto the retina. In a healthy eye, the lens is clear, allowing for sharp vision. However, when proteins in the lens begin to break down, it leads to the cloudiness associated with cataracts.
Deciding to have cataracts surgery is a significant step, often leading to improved vision and a better quality of life. Understanding the journey to surgery can alleviate any anxieties a patient may have.
Cataracts can develop in one or both eyes, though they are not contagious. Initially, they may not significantly impact vision, but as the condition progresses, it can lead to more severe visual impairment. The gradual nature of cataract development often means that individuals may not notice the changes in their vision until they become quite pronounced. This slow progression can sometimes lead to a false sense of security, as many people may attribute their vision changes to normal ageing rather than a specific condition that requires attention.
Common causes of cataracts
There are several factors that can contribute to the formation of cataracts. Age is the most prominent risk factor, with many seniors experiencing some degree of cataract development. However, other factors include:
- Genetics: A family history of cataracts can increase risk.
- Medical conditions: Diabetes and hypertension can elevate the likelihood of cataract development.
- Environmental factors: Exposure to ultraviolet light, smoking, and prolonged use of steroids can also play a role.
Understanding these causes can help in taking preventative measures, although not all cataracts can be avoided. For instance, individuals who are aware of their family history may choose to undergo regular eye examinations to monitor their eye health more closely. Additionally, lifestyle changes such as wearing UV-protective sunglasses, quitting smoking, and managing chronic health conditions can contribute to a lower risk of cataract formation. Awareness of these factors is essential, as they empower individuals to take proactive steps in safeguarding their vision.

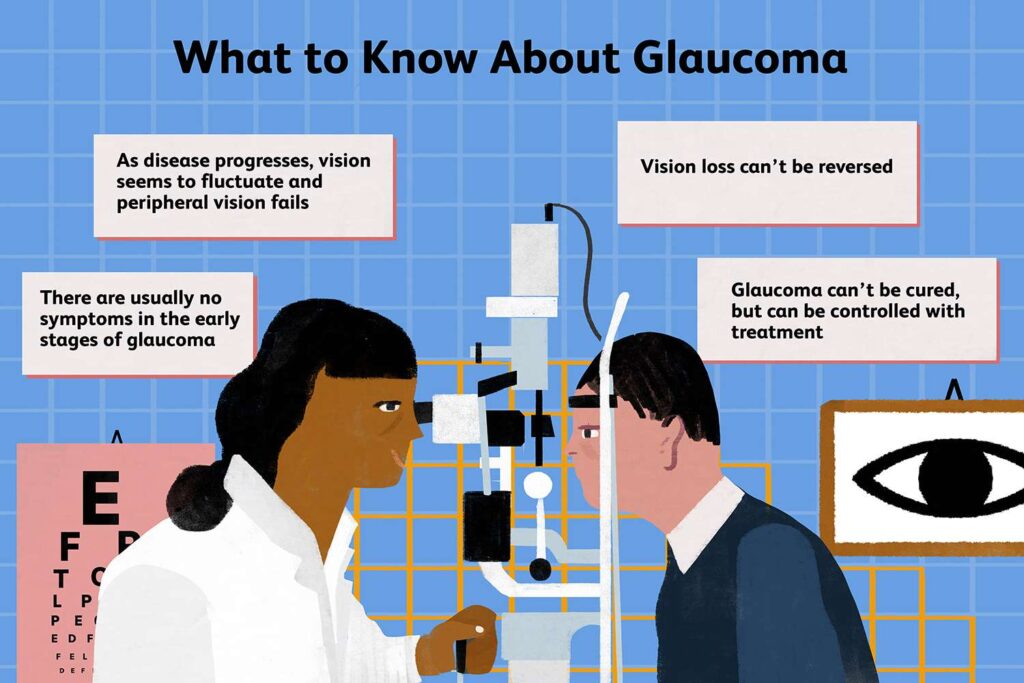
Symptoms and signs of cataracts
People with cataracts may experience a variety of symptoms, which can often lead to a decline in quality of life. The most common signs to watch for include:
- Blurry or cloudy vision
- Difficulties with night vision
- Fading or yellowing of colours
- Glares or halos around lights
Recognising these symptoms early can be crucial in determining the need for surgical intervention. In some cases, individuals may also notice that they need to change their prescription glasses more frequently or that bright lights become increasingly uncomfortable. These changes can be particularly frustrating for those who enjoy activities such as reading or driving, as they may find their ability to engage in these pursuits significantly hampered. Regular eye check-ups become increasingly important as one ages, as they can help detect cataracts and other eye conditions before they lead to more serious complications. Find more about prescription at https://hpi.georgetown.edu/rxdrugs/
The journey to cataracts surgery
When is cataracts surgery necessary?
Surgery is typically recommended when cataracts begin to severely impair daily activities, such as reading, driving, or recognising faces. Each individual’s experience with cataracts varies, so it’s crucial to consult with an ophthalmologist to evaluate the best time for surgery.
Preparing for your cataracts surgery
Preparation for cataracts surgery often begins with a comprehensive eye examination. Your ophthalmologist will assess the extent of the cataract and other factors that may influence surgery, such as your overall health and any concurrent health issues.
Additionally, the doctor may discuss medication adjustments, dietary changes, and logistics for the surgery day, such as arranging transportation post-procedure. Having a clear plan can help mitigate stress and ensure a smoother surgical experience.
The role of your ophthalmologist
Your ophthalmologist is your guide throughout this process. They will provide information, answer questions, and ensure you understand each step of your care. Trusting your ophthalmologist is key; they are there to help you achieve the best possible outcome.
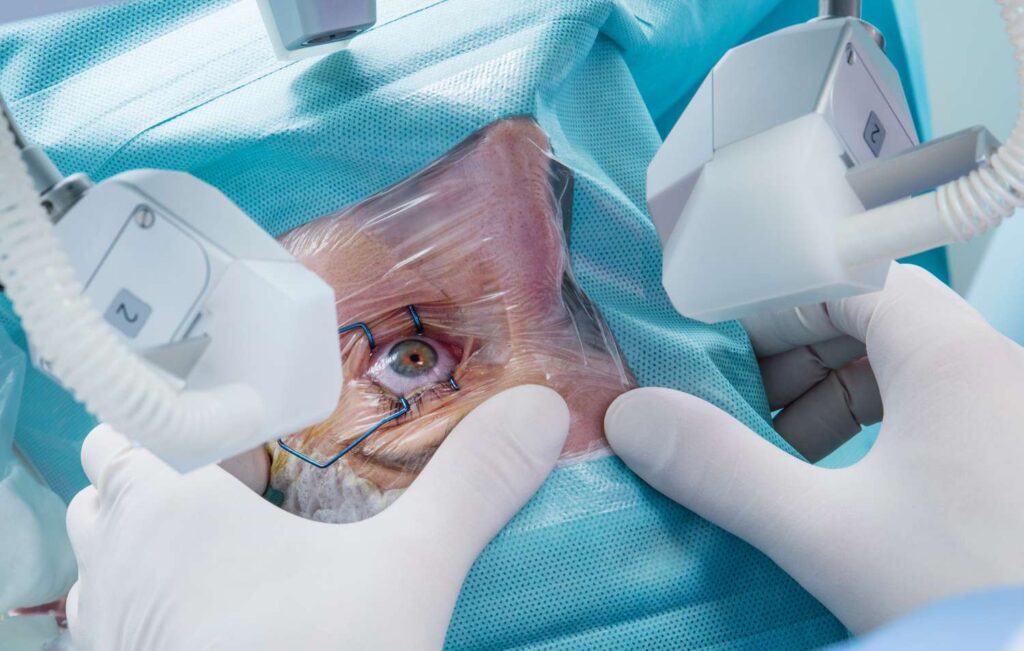
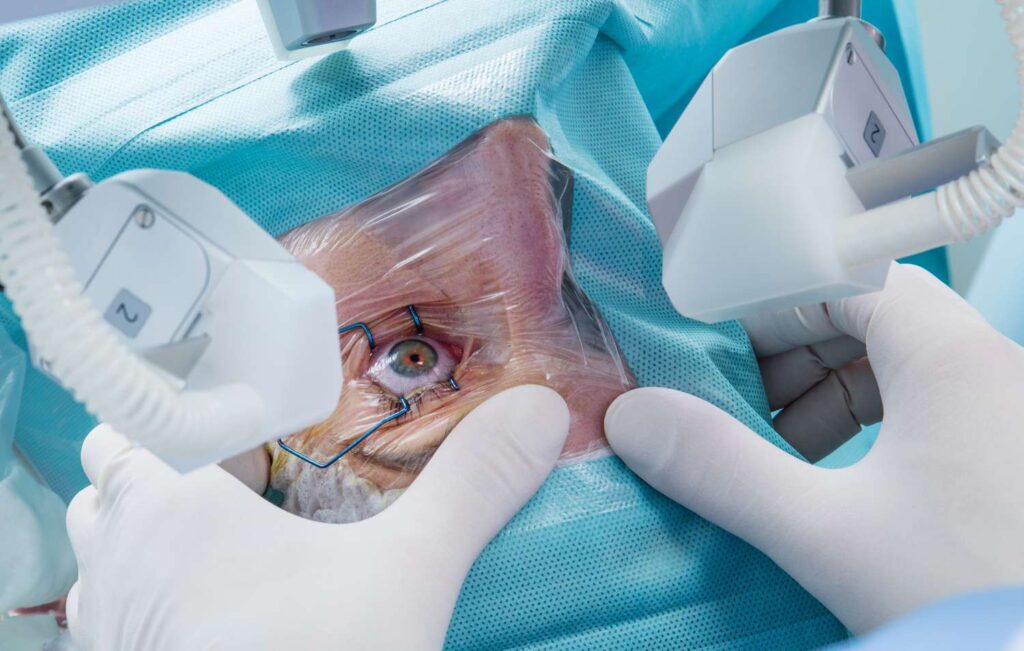
The cataracts surgery procedure
Cataracts surgery is a generally straightforward procedure, but knowing what to expect can ease anxiety for many patients.
What to expect on the day of surgery
The procedure itself usually lasts around 20 to 30 minutes, and most patients can return home on the same day.
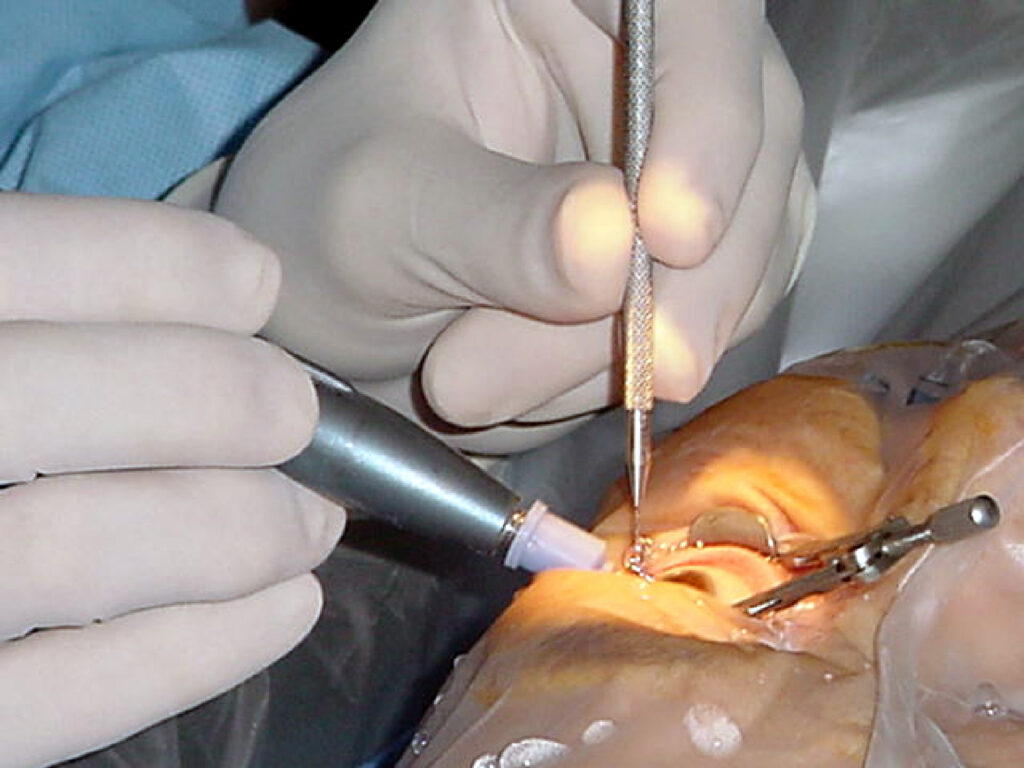
Understanding the surgical process
During the surgery, the cloudy lens is removed, and a clear artificial lens is implanted. This state-of-the-art lens allows for improved vision post-procedure. An ophthalmologist will discuss with you the type of lens best suited to your vision needs.
Post-surgery care and recovery
After the surgery, you will need to follow specific care instructions to ensure optimal healing. It is common to use eye drops and to attend follow-up appointments. It's crucial to avoid strenuous activities and protect your eyes from potential irritants during the recovery phase. To learn more about irritants click here.
Risks and complications of cataracts surgery
While cataracts surgery is considered safe, like any surgical procedure, it comes with potential risks. Being informed about these risks can help patients make educated decisions.
Potential short-term complications
Short-term complications can include infection, inflammation, or bleeding. Fortunately, these issues are rare, and your ophthalmologist will provide instructions on how to minimise these risks effectively.
Long-term risks and how to manage them
Long-term risks may include the development of a secondary cataract, which can cause similar symptoms as the original cataract. Fortunately, this complication can be treated with a simple outpatient procedure called YAG laser capsulotomy.
Regular eye check-ups post-surgery are vital, ensuring any potential issues are addressed quickly and appropriately. By understanding these risks and being proactive about eye health, patients can enjoy successful outcomes.
Other resources: Cataract Surgery restoring Clear Vision with Expert Care