Eye Test for Glaucoma: Why It’s Essential for Early Detection

Glaucoma is a leading cause of irreversible blindness worldwide, making awareness and early detection paramount in preserving vision. Regular eye exams are crucial for identifying glaucoma in its early stages when treatment can be most effective. This article delves into the essential aspects of glaucoma, emphasizing the importance of early detection and the various eye tests required for diagnosis.
Understanding Glaucoma: A Brief Overview
Glaucoma refers to a group of eye diseases that damage the optic nerve, often due to elevated pressure in the eye. This condition can lead to vision loss if not detected and treated promptly. Understanding the intricacies of eye test for glaucoma is vital for effective prevention and management.
What is Glaucoma?
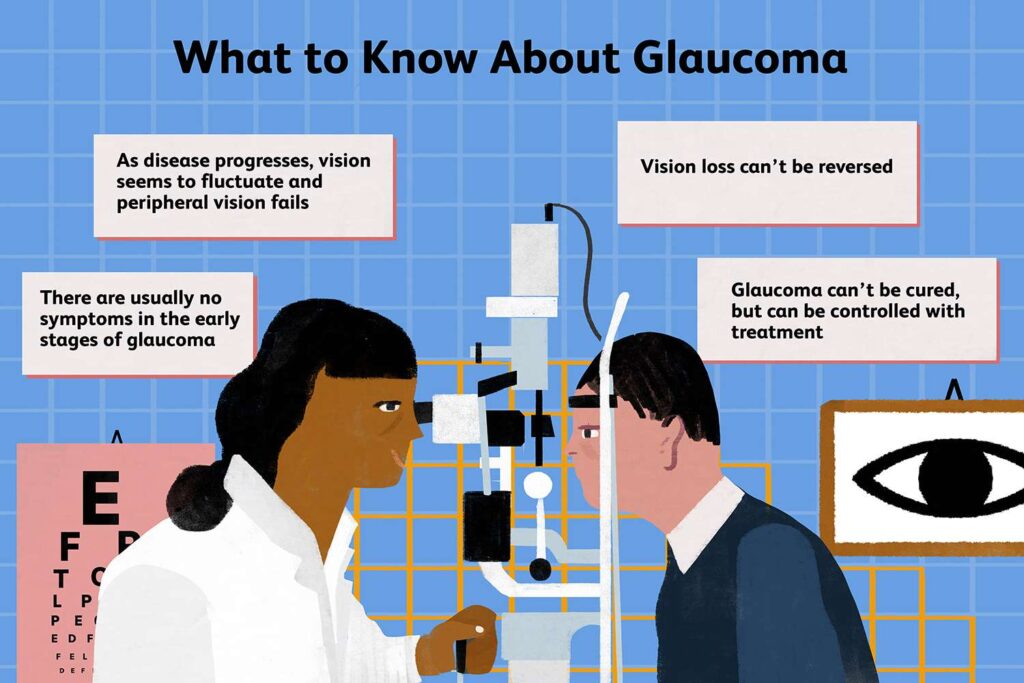
Glaucoma primarily affects peripheral vision and can progress without noticeable symptoms in its early stages. As the optic nerve sustains damage, individuals may experience tunnel vision and, eventually, total blindness. The common misconception that glaucoma only affects the elderly is misleading; individuals of all ages can be at risk. In fact, certain genetic factors and pre-existing medical conditions, such as diabetes or hypertension, can significantly increase one’s susceptibility to developing glaucoma at a younger age. Regular eye examinations become crucial, as they can help detect early signs of the disease before irreversible damage occurs.
Different Types of Glaucoma
There are several types of glaucoma, each with distinct characteristics and risk factors. The most prevalent forms include:
Primary Open-Angle Glaucoma: The most common type, characterized by a gradual progression of vision loss.
Angle-Closure Glaucoma: This type occurs when the peripheral iris blocks the drainage angle of the eye, leading to a rapid increase in eye pressure.
Normal-Tension Glaucoma: Optic nerve damage occurs despite normal eye pressure levels.
Secondary Glaucoma: This can develop as a result of an eye injury, disease, or medication.
Understanding these types can aid in recognizing symptoms and seeking timely intervention. Additionally, lifestyle factors such as diet, exercise, and stress management can play a role in glaucoma management. Studies suggest that a diet rich in antioxidants, particularly vitamins C and E, may help protect the optic nerve. Furthermore, regular physical activity has been shown to lower intraocular pressure, which is a key factor in the progression of glaucoma. Engaging in activities like yoga or tai chi can also promote relaxation and reduce stress, potentially benefiting overall eye health.
The Importance of Early Detection
Detecting glaucoma early is vital for preventing irreversible vision loss. Regular screenings can help identify individuals at risk and allow for prompt treatment, which may significantly delay or prevent disease progression. The American Academy of Ophthalmology recommends that individuals over the age of 40 undergo comprehensive eye exams every two years, and those with a family history of glaucoma or other risk factors should be screened more frequently. Early detection not only protects vision but also empowers patients with knowledge about their eye health, enabling them to make informed decisions regarding their treatment options.
Progression of Glaucoma
Glaucoma often progresses silently; many patients may not notice symptoms until extensive damage has occurred. By the time noticeable vision changes are apparent, significant nerve damage may have taken place. The key to management lies in routine monitoring and active engagement in eye health, especially for those at higher risk. This includes understanding the various types of glaucoma, such as open-angle and angle-closure glaucoma, and recognizing that symptoms can vary widely. Patients should also be aware of the importance of adhering to prescribed treatments, as consistent use of medications can help manage intraocular pressure and slow disease progression. Read more about Glaucoma at https://www.health.harvard.edu/topics/glaucoma
Risks of Late Diagnosis
Late diagnosis of glaucoma can lead to severe consequences, including:
Permanent vision loss that cannot be restored.
Increased healthcare costs associated with advanced treatment options.
Reduced quality of life due to impaired vision.
Individuals diagnosed at an early stage typically have a better prognosis and can maintain a higher quality of life. Furthermore, late-stage glaucoma often requires more invasive procedures, such as surgery, which can come with their own set of risks and complications. The emotional toll of losing one’s vision can also be profound, affecting not just the individual but their families and communities as well. Therefore, raising awareness about the importance of regular eye exams and the risks associated with late diagnosis is crucial in the fight against glaucoma.
Eye Tests for Glaucoma
Several tests are used to diagnose glaucoma and assess the condition of the optic nerve. These tests are designed to evaluate eye pressure and the overall health of the eye.
Comprehensive Eye Exam
A comprehensive eye exam is the first step in assessing eye health. During this exam, an eye care professional will review medical history, conduct visual acuity tests, and perform additional assessments specific to glaucoma. This initial screening is crucial for identifying risk factors. It often includes a discussion about family history, lifestyle choices, and any symptoms the patient may be experiencing, such as blurred vision or halos around lights. Early detection through this thorough evaluation can significantly impact the management and treatment of glaucoma.
Tonometry: Measuring Eye Pressure
Tonometry is one of the key tests used to measure intraocular pressure (IOP). Elevated IOP is a significant risk factor for glaucoma. There are various methods for tonometry, including:
Goldmann Applanation Tonometry: This method is the gold standard for measuring IOP and is performed during a comprehensive eye exam.
Non-Contact Tonometry: Often referred to as the “puff test,” this method uses a quick puff of air to measure eye pressure without contact.
Monitoring IOP can help gauge the risk of developing glaucoma or determine the effectiveness of ongoing treatment. Regular tonometry tests are essential, especially for individuals at higher risk, such as those with a family history of glaucoma or other eye conditions. Understanding the fluctuations in IOP over time can provide valuable insights into the progression of the disease and the response to treatment.
Perimetry: Visual Field Test
Perimetry, or visual field testing, assesses a patient’s peripheral vision. This test is essential because glaucoma often affects side vision first. Patients are asked to look straight ahead and identify when they see lights or objects in their peripheral vision. This test can reveal patterns of vision loss that are characteristic of glaucoma. The results from perimetry can help eye care professionals determine the severity of the disease and tailor treatment plans accordingly. Additionally, advancements in technology have led to automated perimetry, which enhances accuracy and provides a more detailed analysis of visual field loss. To learn more about how visual field testing works click here.
Gonioscopy: Examining the Drainage Angle
Gonioscopy involves examining the drainage angle of the eye using a special lens. This test is critical for determining the type of glaucoma a patient may have. It helps assess whether the angle is open or closed, which influences treatment options. Understanding the anatomy of the drainage angle is vital, as it can affect how fluid drains from the eye and subsequently impact IOP. Gonioscopy can also help identify other conditions, such as angle-closure glaucoma, which requires immediate intervention to prevent vision loss.
Pachymetry: Corneal Thickness Measurement
Pachymetry measures the thickness of the cornea, which is another crucial indicator of glaucoma risk. Studies have shown that thinner corneas can be associated with higher rates of glaucoma. Understanding corneal thickness can help eye care professionals make informed decisions regarding diagnosis and treatment. This measurement is particularly important when interpreting IOP readings, as corneal thickness can influence the accuracy of these measurements. Patients with thinner corneas may require more frequent monitoring and possibly more aggressive treatment strategies to manage their eye health effectively.
Frequency of Eye Tests for Glaucoma
Regular eye examinations are vital for everyone, especially for those at risk for glaucoma. Determining how often to undergo these tests depends on individual risk factors and age.
Recommendations for Different Age Groups
The American Academy of Ophthalmology recommends the following guidelines for routine eye exams:
Adults under 40: Every two to four years.
Adults aged 40-54: Every one to three years.
Adults aged 55-64: Every one to two years.
Adults over 65: Every six to twelve months.

Age-related changes in eye health highlight the importance of adhering to these recommendations to catch potential issues early. For instance, as individuals age, the risk of developing cataracts and macular degeneration also increases, which can complicate the detection of glaucoma. Regular check-ups allow eye care professionals to monitor these changes and adjust treatment plans accordingly, ensuring comprehensive eye health management.
High-Risk Groups: More Frequent Testing
Certain individuals may require more frequent testing, including:
Those with a family history of glaucoma.
Individuals with high eye pressure.
People with other medical conditions like diabetes.
Individuals of African or Hispanic descent, who are at higher risk for developing glaucoma.
For these high-risk groups, it is crucial to maintain vigilant monitoring and engage in proactive discussions with eye care professionals about personalized screening schedules. Additionally, lifestyle factors such as diet, exercise, and smoking can influence eye health and should be considered when assessing risk. For example, a diet rich in antioxidants and omega-3 fatty acids may help support eye health, while regular physical activity can lower intraocular pressure, potentially reducing the risk of glaucoma progression.
In summary, glaucoma is a serious condition that necessitates early detection through comprehensive eye exams and specialized tests. Awareness of the disease, understanding the types, and adhering to recommended testing schedules can significantly impact outcomes and preserve vision. Regular eye tests are not just a recommendation but an essential aspect of maintaining eye health for everyone, especially those at risk for glaucoma. Furthermore, advancements in technology, such as optical coherence tomography (OCT) and visual field testing, provide more precise assessments of eye health, allowing for earlier intervention and better management of glaucoma-related issues.
Related : What Every Patient Should Know About Glaucoma Symptoms and Treatment